Sridhar: Doubtful benefit of isolating discharged COVID-19 patients
The benefit of isolating discharged COVID-19 patients is doubtful, said Siddharth Sridhar, clinical assistant professor in microbiology at HKU, who cited research data from mainland China to support his observation.
Sridar also warned the public that under current government policy, being diagnosed with COVID-19 in Hong Kong now comes with a very very long confinement period.
“Please get vaccinated to protect yourself from COVID-19. Vaccinated people are less likely to catch Delta variant COVID-19 than unvaccinated individuals,” said Sridhar.
Sridhar made the call in the following analysis on his Facebook page posted on 30th October 2021.
Last week, Hong Kong announced new discharge criteria for patients with COVID-19, bringing it in line with the policy of mainland China. One part of the criteria is that patients who test negative for SARS-CoV-2 by consecutive RT-PCR tests will still require 14 days of isolation at the Hong Kong Infection Control Centre (HKICC). This means that anyone diagnosed with COVID-19 in Hong Kong will now have to spend a minimum of 24 days in the hospital and isolation facilities. In reality, hospitalization is likely to be even longer than this for many patients.
The 14-day post-discharge isolation requirement has been a longstanding mainland infection control policy for COVID-19. Early on in the pandemic, Chinese doctors and epidemiologists observed that a proportion of recovered COVID-19 patients became ‘re-positive’ i.e. their RT-PCR tests became positive once again shortly (within 4 weeks) after discharge despite consecutive negative tests at discharge. This phenomenon is quite common and occurred in 10 – 20% of all COVID-19 cases. Several reasons are postulated for this, some of which are:
1) False-negative RT-PCR tests before discharge
2) False-positive RT-PCR tests after discharge
3) Residual non-infectious viral nucleic acids in the upper airway
4) Recrudescence of the infection despite initial recovery
5) Reinfection within short time of recovery
Reasons 4 & 5 above are big concerns because that would mean seemingly recovered patients shed virus and potentially infect others. This led to a fear that these ‘re-positives’ were potentially infectious. Therefore, a system of post-discharge isolation was created in the mainland to detect re-positive patients and subject them to longer medical observation.
Chinese scientists have continued to conduct extensive research into this. So, what are their latest conclusions on the golden question: ‘Are re-positive cases infectious?’
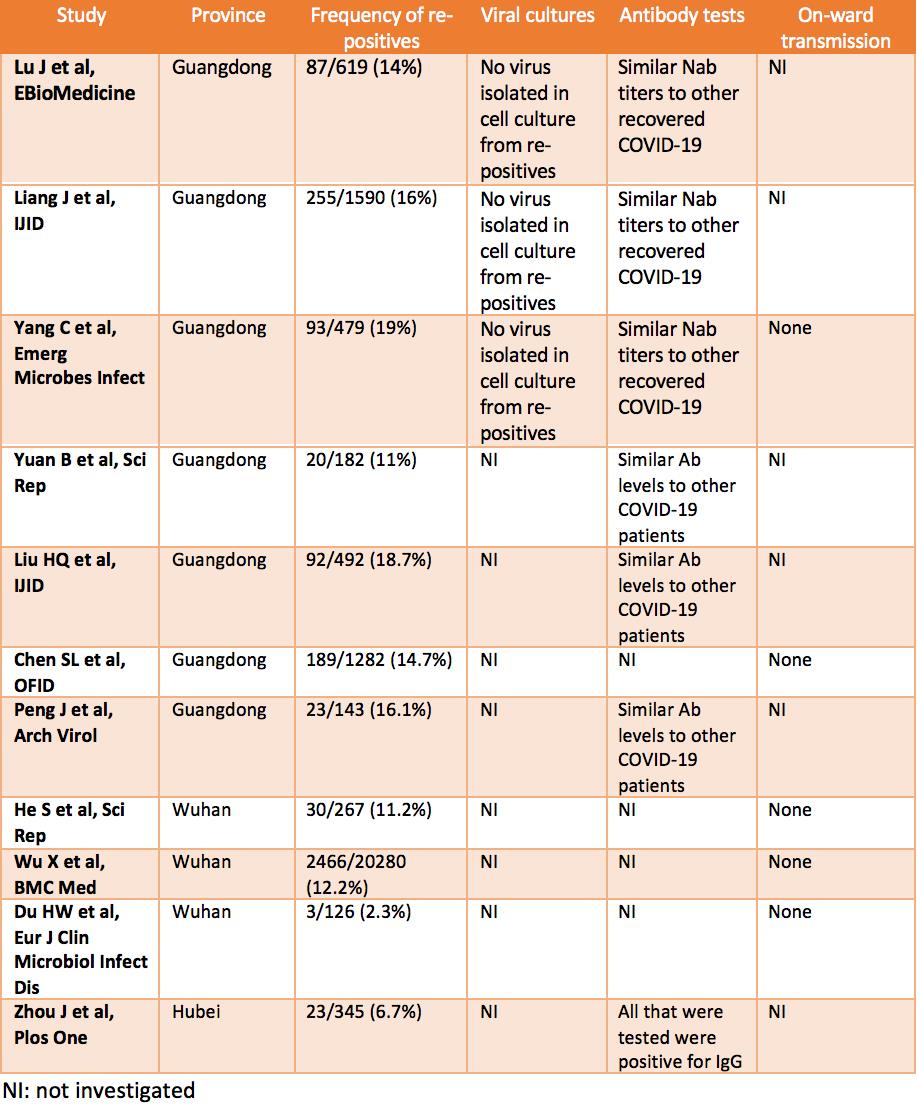
I include some high-quality studies on this topic in the table below. In general, the findings are as follows:
1) ‘Re-positive’ patients generally show improving symptoms and imaging findings;
2) Such patients also have robust antibody responses similar to non-re-positive patients, which indicates that reinfection in such a short time frame is an unlikely cause for them turning re-positive;
3) Their viral loads are low, much lower than the original admission. Studies (Yang C et al, Lu J et al in table below) that attempted next generation sequencing tend to only find genome fragments rather than whole genomes, which would indicate non-infectious viral nucleic acid rather than complete viral particles;
4) Studies that attempted cell culture fail to recover any infectious virus from re-positive patient samples;
5) Most importantly, epidemiological studies (Yang C et al and Chen SL et al in table below) failed to find any onward transmission from re-positive patients to close contacts.
I quote the following conclusions verbatim from some of the studies:
1) “Recurrent positive patients pose a low transmission risk, a relatively relaxed management of recovered COVID-19 patients is recommended.” Yang C et al, Emerg Microbes Infect, study by Shenzhen CDC
2) “Re-positive SARS-CoV-2 cases do not appear to be caused by active reinfection and were identified in ~14% of discharged cases. A robust NAb response and potential virus genome degradation were detected in almost all re-positive cases, suggesting a substantially lower transmission risk, especially through respiratory routes.” Lu J et al, EBioMedicine, study by Guangdong CDC
3) “The viral load in re-positive cases was very low; patients were not infectious and the risk of human-to-human transmission was extremely low.” Liang L et al, IJID, study by Guangdong CDC
4) “Our data suggest that the short-term recurrence of positive SARS-CoV-2 RNA in discharged patients is not a relapse of COVID-19, and the risk of onward transmission is very low.” Chen SL et al, OFID, study from universities in Guangdong
5) “This retrospective study in Wuhan analyzed the basic characteristics of recovered COVID-19 patients with re-positive PCR test and found that these cases may not be infectious.” Wu X et al, BMC Medicine, study from Wuhan CDC & others
Note that the above applies to immunocompetent patients. Some immunocompromised are known to harbor potentially infectious COVID-19 for long periods of time (although they would not be expected to test negative and then re-positive).
Furthermore, there is no 100% certainty in science and short-term re-infection is theoretically possible although extremely uncommon (Abu-Raddad LJ et al, Clin Infect Dis). One case report from Portugal claims that a re-positive healthcare worker infected others (Correia AM et al, IJID) although there are uncertainties in the interpretation of the study. But, on the whole, these large studies published from China strongly indicate that the vast majority of re-positive patients are not infectious.
Therefore, the benefit of post-discharge isolation of COVID-19 patients to public safety is doubtful. This policy is also difficult to sustain when Hong Kong faces an inevitable future wave of COVID-19. Unlike the mainland, we do not have unlimited land and manpower resources for quarantine facilities when there is a large local outbreak (and such resources are probably better prioritized elsewhere anyway).
In any case, please note that being diagnosed with COVID-19 in Hong Kong now comes with a very very long confinement period. Please get vaccinated to protect yourself from COVID-19. Vaccinated people are less likely to catch Delta variant COVID-19 than unvaccinated individuals.