The risk of Covid-19 re-infection
Siddharth Sridhar, clinical assistant professor from HKU ’s Department of Microbiology shared his insights on the risk of Covid-19 re-infection in an article published on his Facebook on 22 August, 2020. Below is the full article.
Can you catch COVID-19 twice?
This question has received a lot of attention. There is fear that immune responses to SARS-CoV-2 infection are weak and temporary, putting millions at risk of re-infection. We have recently heard reports of a young patient in Hong Kong who, on prima facie evidence, appears to have caught COVID-19 twice.
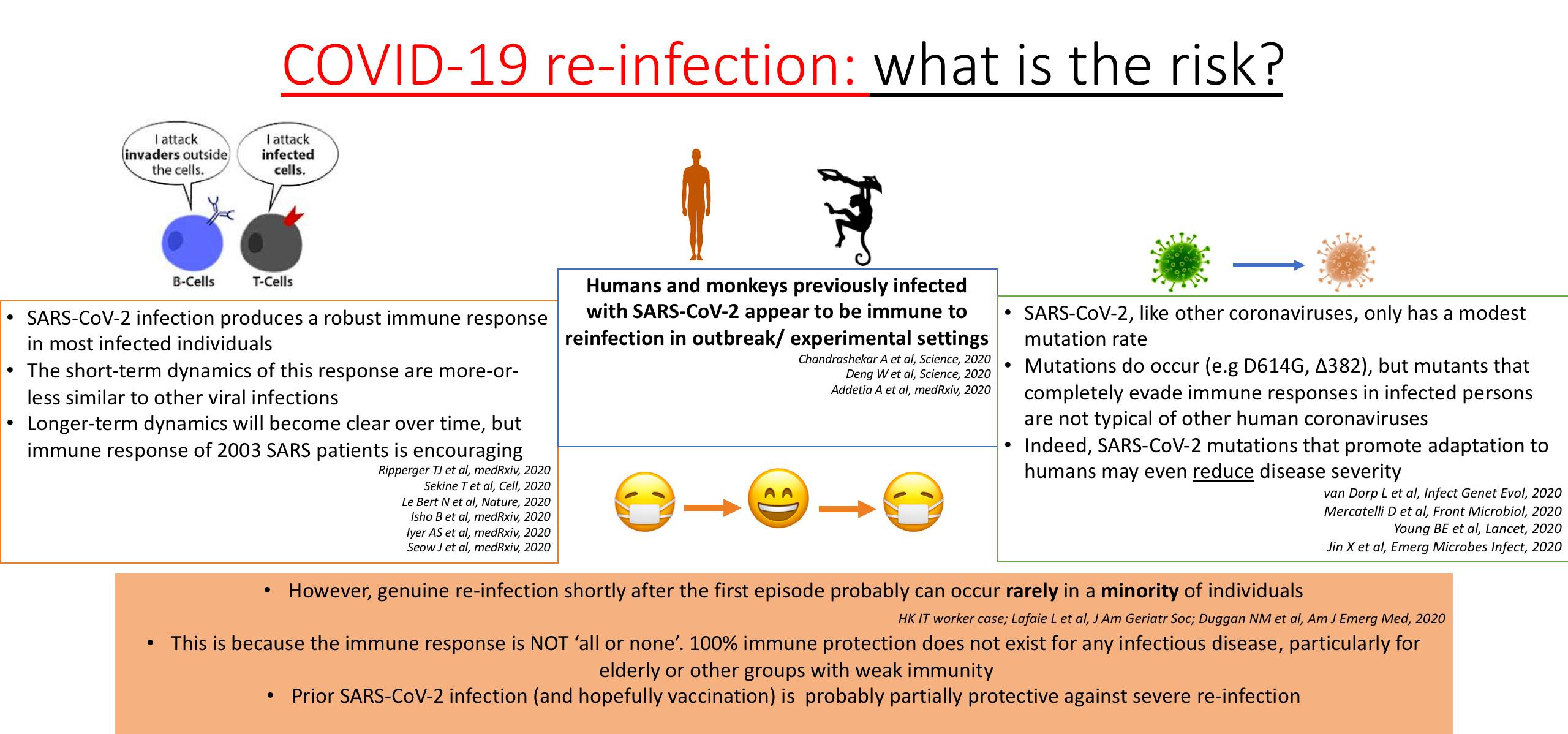
So, what do we know about this? I describe the current evidence on this below. Due to the length of the post (sorry!), references for these points are included in the attached infographic.
1. Most people develop a robust immune response after COVID-19 infection. This response is marked by a surge in antibodies, which then decline to a new baseline as the patient recovers. This response is fairly typical of the body’s response to other viral infections.
2. Some asymptomatic or mildly infected COVID-19 patients have weak antibody responses that decline rapidly, but they still mount a strong ‘T-cell’ response. These T-cells are a critical part of the immune system that we cannot conveniently measure in ordinary labs (unlike antibodies).
3. We know that this immune response persists for at least 3 – 5 months, which is the maximum possible period of observation in studies so far. However, longer-term immunity is entirely possible based on observations in 2003 SARS patients, but will require confirmation from more studies down the road.
4. Does this immune response protect against a second COVID-19 infection? In experimentally infected monkeys and in the Seattle fishing boat study, the answer is YES. Having an immune response against SARS-CoV-2 definitely appears to reduce chances of getting symptomatic re-infection.
5. But what if the virus mutates? Yes, mutations certainly occur, but coronaviruses mutate somewhat less frequently than other RNA viruses. Mutants with complete evasion of host immunity are extremely unusual in the human ‘common cold’ coronaviruses (NL63, 229E, HKU1 and OC43). Most SARS-CoV-2 mutants, including the famous D614G, are not predicted to radically alter the immunogenicity of SARS-CoV-2. Even if they do alter it somewhat, prior exposure is expected to confer some degree of protection.
6. So, the golden question, what is the risk of SARS-CoV-2 re-infection? Based on the above evidence, for most individuals, the first episode of COVID-19 confers a robust immune response, which is likely to be protective against severe symptomatic re-infection, at least in the short term. Genuine re-infection shortly after the first episode is still possible, but is uncommon. The reason why it is still possible is that the human immune response is not ‘all or none’. Instead, it confers a spectrum of protection. In some individuals, such as the elderly, the response tends to be weaker with ‘blind spots’, leading to a chance of re-infection. Such blind spots may be sporadic or due to subtle underlying immune abnormalities.
7. My prediction is that SARS-CoV-2 will permanently circulate in human populations as a new respiratory virus with low death-rate as more and more individuals have some degree of protection (either by natural infection or vaccination). Our amazing immune systems will adapt to this virus and deal with it (hopefully with a bit of help from vaccines).



